Periodontal Disease
Periodontal diesease is an infection that affects the tissues and bone that support teeth.
Healthy gum tissue fits like a cuff around each tooth. When someone has periodontal disease, the gum tissue pulls away from the tooth. As the disease worsens, the tissue and bone that support the tooth are destroyed. Over time, teeth may fall out or need to be removed. Treating periodontal disease in the early stages can help prevent tooth loss.
How do I know if I have periodontal disease?
It can be hard to know. You can have periodontal disease without clear symptoms. That's why regular dental checkups and periodontal examinations are very important.
Several warning signs can signal a problem. If you notice any of the following, see your dentist:
- gums that bleed when you brush or floss
- red, swollen, or tender gums
- gums that have pulled away from your teeth
- bad breath that doesn't go away
- pus between the teeth and gums
- loose or separating teeth
- a change in the way your teeth fit together when you bite
- a change in the fit of partial dentures
What causes periodontal disease?
Periodontal disease is caused by plaque, a sticky film that is always forming on your teeth. Plaque contains bacteria that produce harmful toxins. If teeth are not cleaned well, the toxins can irritate and inflame the gums.
Inflamed gums can pull away from teeth and form spaces called pockets. The pockets provide a home for more bacteria. If the infected pockets are not treated, the disease can get worse. The bone and other tissues that support teeth are damaged.
Plaque can be removed if you brush your teeth twice a day and floss (or use another between-the-teeth cleaner) daily. If plaque stays on teeth, it can harden into a rough surface called tartar. Tartar can only be removed when teeth are cleaned at the dental office.
How can I prevent periodontal disease?
A good oral hygiene routine practiced for a few minutes twice a day can help reduce your risk of getting periodontal disease and tooth decay.
Are you at risk?
- People who smoke or chew tobacco are more likely to have periodontal disease.
- Diseases that affect the whole body--such as diabetes, blood cell disorders, HIV infections, and AIDS--can lower resistance to infection, making periodontal disease more severe.
- Many medications--like steroids, some anti-seizure drugs, cancer therapy drugs, blood pressure drugs and birth control pills--can affect the gums. Some medications have side effects that reduce saliva. A lack of saliva can result in a constant dry mouth, which can irritate soft tissues. Tell your dentist about all your medications and any changes that occur in your health.
- Teens, pregnant women, and those taking birth control pills face changes in the body's hormone levels. These changes can cause gum tissue to become more sensitive to the toxins produced by bacteria.
- Genes may play a role.
- The bacteria associated with periodontal disease may be passed from parents to children and between partners. Research suggests that the bacteria that cause periodontal disease can be passed through saliva.
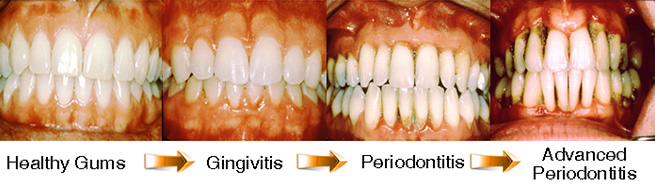
Types of periodontal diseases
There are many types of periodontal diseases. People of all ages can be affected, from children to seniors.
Gingivitis is the mildest form of periodontal disease. It causes the gums to become red and swollen and to bleed easily. There is usually little or no discomfort at this stage. Gingivitis can be reversed with treatment in the dental office and good oral care at home.
Chronic Periodontitis is a form of periodontal disease that results in swelling and redness in the tissues around the teeth. Patients suffer loss of tissue and bone that may become more severe over time. In chronic periodontitis, pockets form and/or gum tissue pulls back. This is the most common form of periodontitis in adults but can occur at any age. It usually gets worse slowly, but there can be periods of rapid progression.
Aggressive Periodontitis is a highly destructive form of periodontal disease that occurs in patients who are otherwise healthy. Common features include rapid loss of tissue and bone. This disease may occur in some areas of the mouth, or in the entire mouth.
Periodontitis as a Manifestation of Systemic Disease is a form of periodontitis that is the result of a specific disease or disorder. Patients who have certain blood diseases or genetic disorders frequently show signs of periodontal disease.
Necrotizing Periodontal Diseases results in the death (or necrosis) of tissues surrounding the tooth and connecting bone. This most commonly comes with pain, bleeding, and a foul odor. These infections can partly be caused by stress, tobacco use, malnutrition, and HIV infection.
Stages of Periodontal Diseases
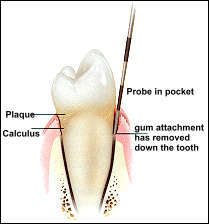
Checking for Periodontal Disease
During your dental checkup, the dentist or hygienist examines your gums. A periodontal probe is gently used to measure the depth of the pockets surrounding each tooth. When teeth are healthy, the pocket depth is usually three milimeters or less. The periodontal probe can indicate whether you have developed any pockets and the depth of those pockets. Generally, the more severe the disease, the deeper the pocket.
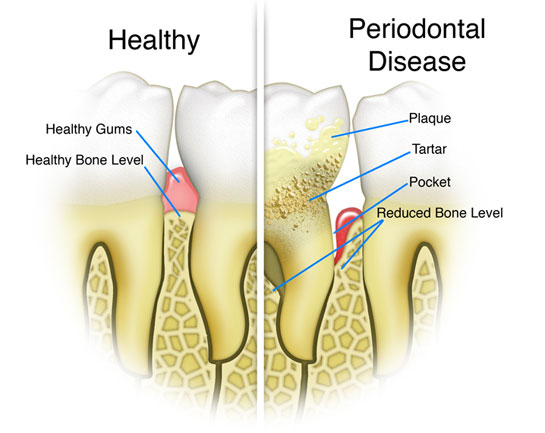
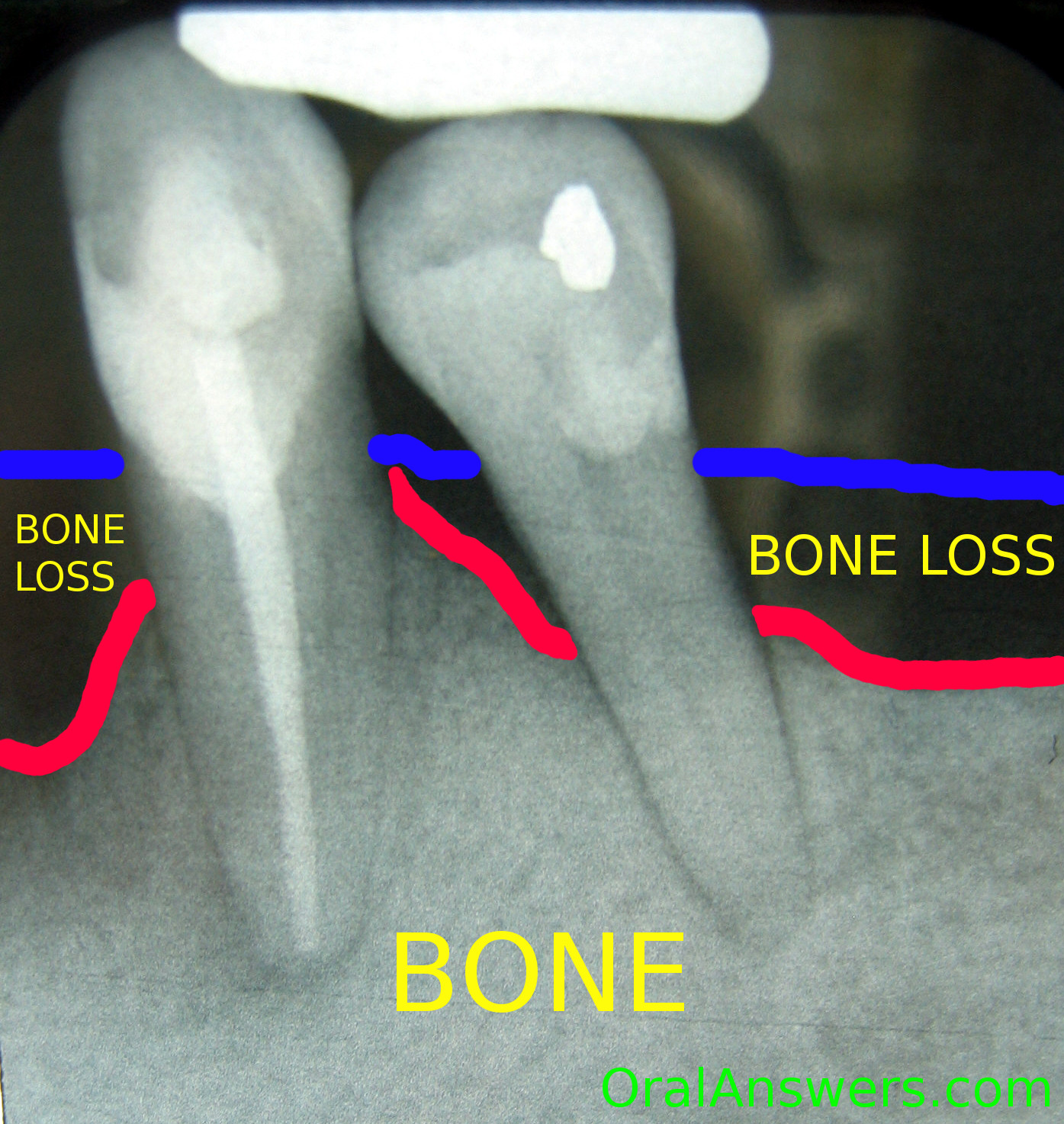
Dental X-rays usually are taken to check the amount of bone supporting the teeth and to find other problems not visible during the clinical exam. If periodontal disease is diagnosed, the dentist may provide treatment or may refer you to a periodontist (a dentist who specializes in the prevention, diagnosis, and treatment of periodontal diseases).
Treating Periodontal Diseases
Peridontal treatment methods depend upon the type and severity of the disease. IF the disease is caught very early (when it is gingivitis), and no damage has been done to the supporting structures under the teeth, you may simply have a professional cleaning and be given instructions on improving your daily oral hygiene.
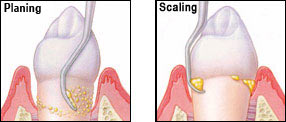
Even with these measures, some patients develop more severe periodontal disease that must be treated. The first step usually involves a special cleaning, called scaling and root planing. In this treatment, plaque and tartar are carefully removed down to the bottom of each periodontal pocket. Part of this procedure includes smoothing the tooth's root surfaces to allow the gum tissue to heal and reattach to the tooth. This is sometimes also called "periodontal cleaning" or "deep cleaning" and may take more than one visit.
Your dentist also may recommend medicines to help control infection and pain, or to aid healing. These medicines could include a pill, a mouthrinse, or a substance that the dentist places directly in the periodontal pocket after scaling and root planing. Your dentist may also stress the need to stop using tobacco and to control any related systemic disease, like diabetes.
At your follow up visits, the dentist or hygienist measures the pocket depth again to check the effect of the scaling and root planing. If the disease continues to advance to the point where the periodontal pockets deepen and the supporting bone is lost, more treatment may be necessary. You may be referred to a periodontist.
Periodontal Surgery
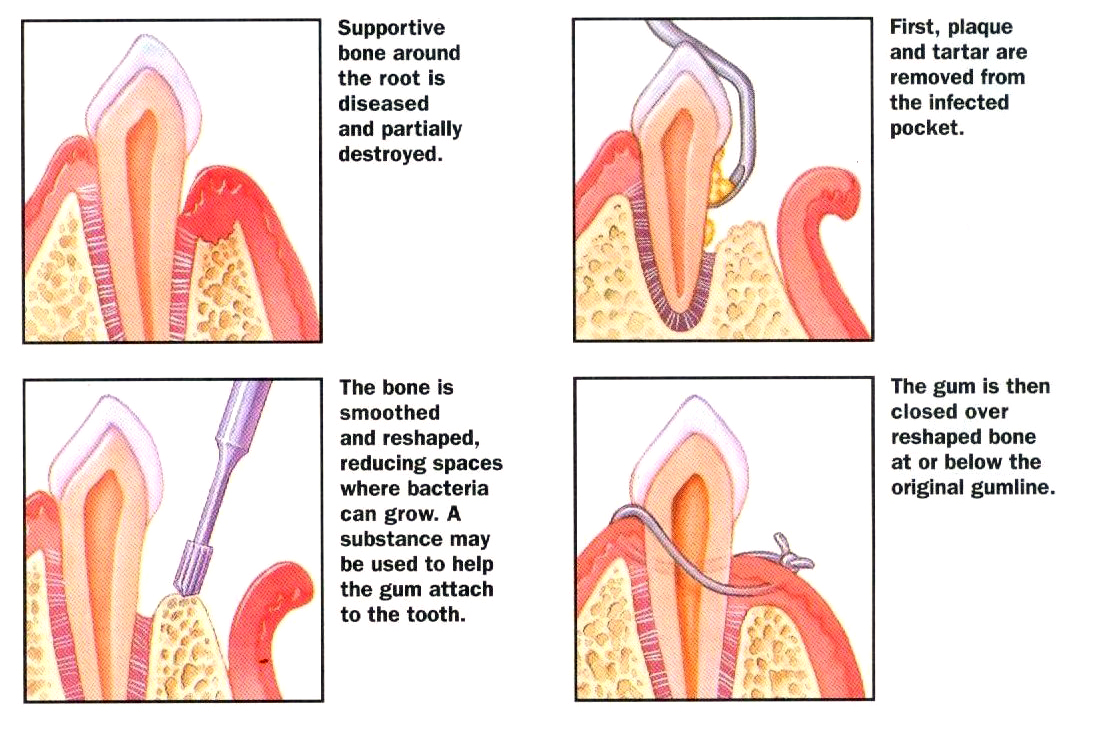
When deep pockets develop, it is difficult to completely removed plaque and tartar even with careful oral hygiene. If the pockets do not heal after scaling and root planing, periodontal surgery may be needed to reduce the pocket depth and make teeth easier to keep clean.
Surgery allows the dentist to get to hard-to-reach areas that require the removal of tartar and plaque. The gums are stitched back into place or into a new position to make tissue snug around the tooth.
If bone has been destroyed by periodontal disease, bone surgery may be needed to rebuild or reshape bone destroyed by periodontal disease. Splints, bite guards or other appliances may be used to hold loose teeth in place and to help tissue heal. If too much gum or bone tissue has been lost, a gum or bone graft may be performed.
Sometimes a membrane layer is placed at the surgical area to help the gum tissue stay in place while the tooth root re-attaches to the supporting ligament. This is called guided tissue regeneration. After healing, the membrane dissolves or is removed. After surgery, the dentist may apply a protective dressing over teeth and gums and a special mouthrinse may be recommended or prescribed. An antibiotic and pain reliever also may be prescribed.
Care After Treatment
Once your periodontal treatment is completed, your dentist may recommend more frequent checkups. Regular dental visits and deep cleanings are important to keep periodontal disease under control. In some cases, your appointments may alternate between your general dentist and a periodontist.
Good oral hygiene at home is also important to help keep periodontal disease from becoming more serious or from coming back. It just takes a few minutes twice a day to care for your teeth and gums. Daily cleaning helps keep the plaque under control and reduces tartar buildup.
If you use tobacco, ask your dentist or physician for information about how to successfully stop the habit. Tobacco contains chemicals that can slow the healing process and make the treatment results less predictable.
You don't have to lose teeth to periodontal disease. Brush, clean between your teeth, eat a balanced diet, and schedule regular dental visits for a lifetime of healthy smiles.
--From America Dental Association 2011--